View this testimony as a PDF here.
Recommendation:
Restore a system of modest grant support for Community-Based Organizations to boost Texas Medicaid’s ability to connect more eligible children and moms to health coverage, especially in rural and small-town Texas. The House Select Committee has endorsed this policy in its interim report.
- Texas has seen big results when we invest in outreach for Medicaid and the Children’s Health Insurance Program (CHIP). The 2000 CHIP roll-out was Texas Medicaid’s first-ever outreach effort. Texas broke national records enrolling children in our new CHIP program in 2000 and 2001 with help from a strong intentional plan for marketing, outreach, and enrollment assistance.
- Grants were available in the 2000s for community-based outreach and enrollment assisters. Those early programs have since been replaced by HHSC’s Community Partners Program (CPP), which provides important training resources, but no longer offers local and regional grants that can make offering outreach and enrollment help possible in smaller towns and rural counties. Grants to support a dedicated computer for enrollment, broadband connection, and ability to print forms and flyers can make it possible for smaller clinics, health centers, and other CBOs to play a big role in their area getting children signed up and renewed. Every Texan and the Children’s Health Coverage Coalition (CHCC) believe that this recommended renewed budget investment will expand the reach of the CPP to reach more under-resourced parts of Texas.
Texas Needs More Hands on Deck
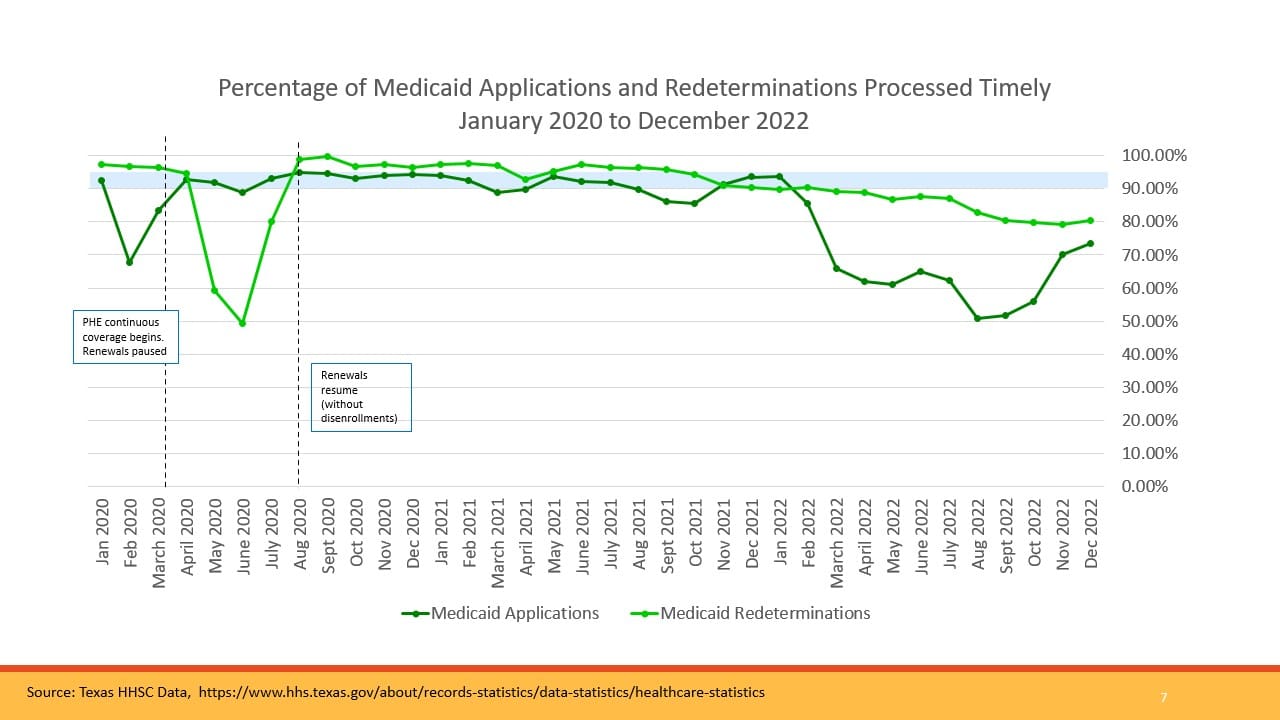
- Texas Medicaid has had big delays and backlogs in processing applications and renewals throughout 2022, with numbers slowly improving but still not up to federal law standards.
- Texas HHSC must start recertifying all Medicaid enrollees in April 2023, as Congress ends the pandemic-related Medicaid continuous coverage. Because so many have gone since 2020 without a renewal, HHSC needs extra help getting client contact information updated (including lost passwords, locked online accounts) so that eligible Texans—mostly children—don’t lose coverage for which they are qualified.
- Texas HHSC Eligibility offices were closed in 2021 and 2022 in Austin (houses staff but no longer public facing); Brownfield; Post; Port Lavaca; Fredericksburg; Kirbyville; Ennis; and Odessa. Texas HHSC’s largest eligibility offices — Telephone Road in Houston—closed in August 2022 for repairs “with no anticipated reopening date.”
Outreach/Application Help to Reduce Texas’ Worst-in-the-Nation Child Uninsured Rate
- The percentage and numbers of uninsured Texas children grew from 2017 to 2019, and Texas children’s Medicaid and CHIP enrollment dropped in 2018 and 2019. The number of uninsured Texas children declined during the COVID-19 pandemic due to the federal pandemic Medicaid continuous coverage policy that expires March 2023.
- Texas children and youth (under 19) in 2021 are more than twice as likely as U.S. kids overall to be uninsured: 11.8%, compared to 5.4% for the U.S. Only one other state (WY) has a child uninsured rate in double digits. Texas’ last-place rank is despite our child uninsured rate improving from 12.7% in 2019.
- Nearly 930,000 Texas children were uninsured in 2021, and the Census estimates 495,000 of those had incomes below two times the Federal Poverty Income Level. 16% of Hispanic Texas children were uninsured, compared to 8% of non-Hispanic white children lacking coverage.
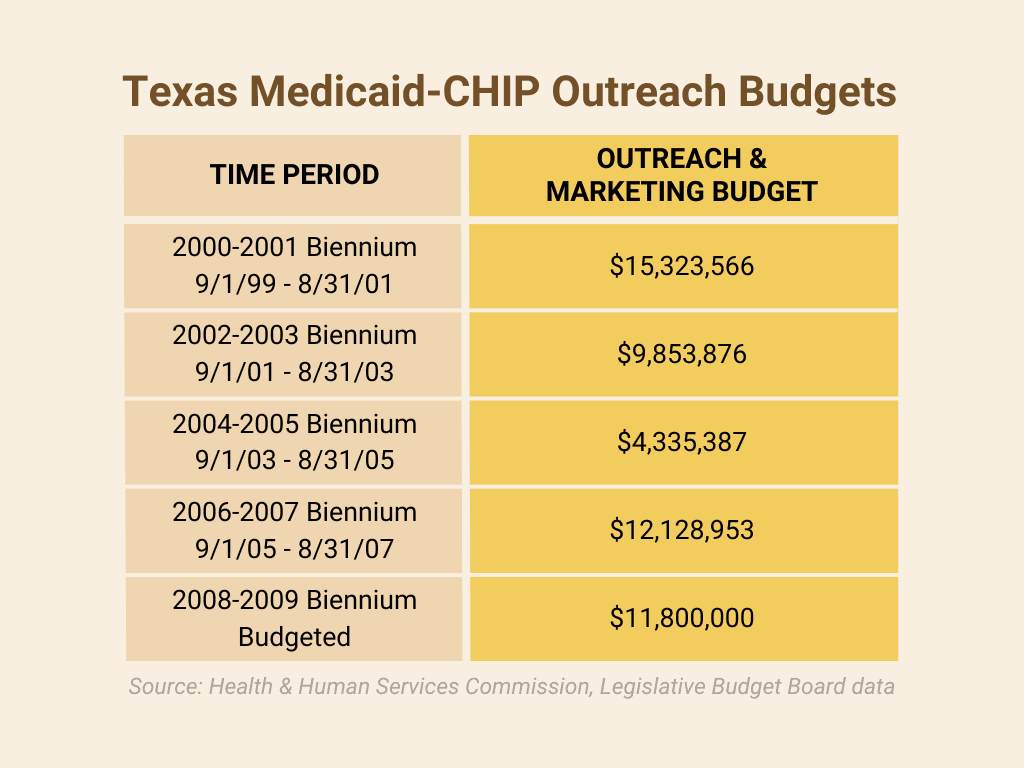
Funding to Restore Community-Based grants for the Community Partners Program
Every Texan and The Children’s Health Coverage Coalition (CHCC) strongly urge the Legislature and HHSC to allocate an amount that—at minimum—restores Texas’ original biennial investment for the 2000-2001 biennium ($15.3 million) in outreach and application assistance.
Texas’ investment should:
- Meet the current need to reduce the number of eligible-but-uninsured children;
- Take into account the historical funding in 2000-2001, population growth, and inflation. Texas’ child population has increased by one-third (33%) from 5.9 million to 7.9 million from 2000 to 2021.
- Help Texas Medicaid to manage the “unwinding” of COVID-19 Medicaid continued coverage, without a loss of children’s coverage in Medicaid, CHIP, and private Marketplace coverage.
A modest investment in outreach and assistance will reduce state staffing costs, reduce uninsured rates among children, and support the continued quality and improvement of Texas’ eligibility systems.
Relevant statutory citations: Health & Safety Code Sec. 62.056. COMMUNITY OUTREACH CAMPAIGN; TOLL-FREE HOTLINE. Government Code Sec. 531.752. ESTABLISHMENT OF COMMUNITY-BASED NAVIGATOR PROGRAM.
Other States: Information voluntarily provided by some states in CHIP Annual Reports show that states including Iowa, Virginia, and Wyoming support both local outreach assisters and school-based outreach and enrollment.
For additional information, contact Anne Dunkelberg at dunkelberg@everytexan.org, Karla Martinez at kmartinez@everytexan.org, or Stacey Pogue at pogue@everytexan.org.