Archives
1) What is the new Public Charge rule?
It’s a new U.S. Department of Homeland Security rule that will make it harder for people to go through the lawful immigration process and get a green card (also known as Lawful Permanent Resident status or LPR). The rule governs under what conditions immigration authorities can turn down a person’s application for lawful immigration status. Specifically, the rule allows denial of a person’s application if they would rely too much on government support, what historically was known as being a “public charge.”
Since 1999, only two public benefits would bar a prospective immigrant: (a) total reliance on government cash assistance or (b) total reliance on government institutional care (such as a nursing home). But the federal administration wants to make big changes.
2) The new public charge rule is NOT in effect.
Federal officials released a proposed federal rule change for public comment in October 2018, and a modified “final” version was published 8/14/2019. That rule was scheduled to take effect on 10/15/2019, but five different courts issued injunctions that stopped the rule from taking effect, and three of those injunctions are nationwide. So, the rule has not taken effect, and “old” 1999 policies are still in force.
At present, there is no way to know how long we will wait before a decision is final. The courts could completely stop the rule, or it could take effect someday in the future.
3) Who would be affected?
Narrowly, the public charge rule applies to any immigrant trying to get a green card (Lawful Permanent Resident status), or any person seeking a visa to enter the U.S. from another country.
4) Many types of immigrants would not be affected.
The public charge test does NOT apply to:
- Lawful Permanent Resident status (green card holders) applying for citizenship
- Refugees and asylum seekers
- Several humanitarian categories, including Violence Against Women Act (VAWA) petitioners, domestic violence and human trafficking survivors (U or T visa)
- Special Immigrant Juvenile status (used for children in foster care)
If the proposed rule ever does take effect in the future: Items 5-10 below explain the potential effects
5) What would the new rule change?
Since 1999, only (a) total reliance on government cash assistance or (b) total reliance on government institutional care (such as a nursing home) would exclude a prospective immigrant.
The new rule is much more restrictive. If the rule ever takes effect, the “public charge test” would also consider whether the applicant has used, or is likely to use specific benefits in the future. These are: Federal, state, local and tribal Cash Assistance; Supplemental Nutrition Assistance Program (SNAP, formerly known as food stamps); Public Housing or Section 8 Housing Vouchers and Rental Assistance; or adult Medicaid.
IMPORTANT:
- Medicaid use for emergency services, for pregnant women and new mothers, or for children under age 21 will not count against immigration applicants.
- Only the benefits listed above would be added to the Public Charge test if the new rule takes effect. No others (not the Women, Infants and Children (WIC) Program, the Children’s Health Insurance Program, school meals, Head Start, etc.)
The rule would give preference to wealthier, more educated immigrants, and penalize lower-income, less-educated, or less-healthy immigrants. Applicants would have a harder time getting through the lawful immigration process if they have a family income below 250 percent of the federal poverty income, which in 2019 is less than $65,000 a year of income (pre-tax) for a family of four. Immigration officials will also consider the green card applicant’s positive or negative “totality of circumstances “including the applicant’s age, health, family status, education, job skills, and assets.
6) The new rule does NOT look at whether a family member has used public benefits, only benefits used by the individual applicant.
Early drafts of the proposed rule did propose to hold the use of public benefits by a U.S. citizen child against a parent’s green card application, so this is a very important change, and many Texas families may not have this information. This means that it will NOT benefit a green card applicant to have their U.S. citizen or green card holding family members drop their own SNAP, Medicaid, or housing benefits.
Fear of using benefits is widespread, however, even for U.S. citizen family members. It is critical that Texans spread the word that immigrants’ family members should continue using their important public benefits. Many families have already been scared into dropping important benefits. Both Children’s Medicaid and SNAP (food stamps) have seen significant enrollment drops.
7) If the new rule took effect, the public charge test would look at the green card applicant’s use of benefits (a) AFTER the rule took effect, and (b) also guess at the applicant’s likely FUTURE use of the newly listed benefits.
Immigration authorities would only take SNAP, adult Medicaid, or housing benefits used by the applicant on or after the effective date into account. The only exception is cash assistance or long-term care benefits because they were already considered under the “old” public charge rule.
Once the rule takes effect, an applicant who has used SNAP, Medicaid, or housing benefits for a combined total of 12 months out of any 36-month period will have that use considered “a heavily weighed negative factor” in deciding whether someone is likely to become a public charge. Receiving two of these programs, such as SNAP and Medicaid, in a single month, will be counted as two months. Again, it’s important to note that their own use of Medicaid for emergency services, for pregnant women and new mothers, or for children under age 21 will not count against immigration applicants.
8) Simple answers are not always possible, and the rule affects more Texans than just green card and visa applicants.
One example of the complexity that adds to community fears: The U.S. has different policies for immigrants whose green card interview is inside the U.S. (through the Dept. of Homeland Security) versus those having the interview outside the U.S. (through U.S. Dept. of State consulates). That means we cannot give mixed-status families a simple “use of benefits by your family members won’t affect your legal immigration.” Instead, we must say that it depends on whether the individual seeking the green card is interviewing for a green card inside or outside the U.S. (for the time being).
As a practical matter, just the threat of the new rule has already affected many more Texans than just those with active green card applications. Unfortunately, many other immigrants—including Lawful Permanent Residents and others—fear that use of benefits for health care, housing, or hunger prevention by their family members who are U.S. citizens or who already have their own green card (LPR status) will hurt the applicant’s ability to get a green card, or will stop a green card holder from becoming a U.S. citizen. This is misinformation. This fear has put whole families at risk of neglecting basic needs to be healthy, successful in school and productive, in order to keep the family united.
9) How many Texans may be affected?
The numbers are sobering: 5.6 million Texans live in a family that includes at least one non-U.S. citizen (of any immigration status). Because of the fear spreading through families where any family member is not a U.S. citizen, all of these 5.6 million Texans could somehow be affected.
- About 1.9 million of these are kids age 17 or younger, of whom the great majority—about 1.65 million—are U.S. citizen children. That’s more than one in every four Texas children.
- 3.9 million of those Texans have family incomes targeted by the new rule (under 250 percent of the federal poverty income), which in 2019 is less than $65,000 a year pre-tax income for a family of four.
A growing body of national research and Texas tracking shows that many families have already dropped benefits (including for children).
10) Immigration legal assistance agencies and lawyers can help.
Many families are exempt from the public charge rule but may need a qualified and trusted expert to accurately advise on that. Free and low-cost help is available to understand whether the rule affects a specific person or family. Organizations across Texas can either provide legal advice to applicants who are subject to the rule or refer them to other qualified immigration attorneys. Find a statewide list of Texas immigration legal services providers.
The Center for Public Policy Priorities and Children’s Defense Fund–Texas are partnering to make technical assistance and support available to organizations, local governments, institutions who need access to reliable information for training, and for community education. Here are slides and background resources with more information. Email dunkelberg@cppp.org or canderson@childrensdefense.org for more information.
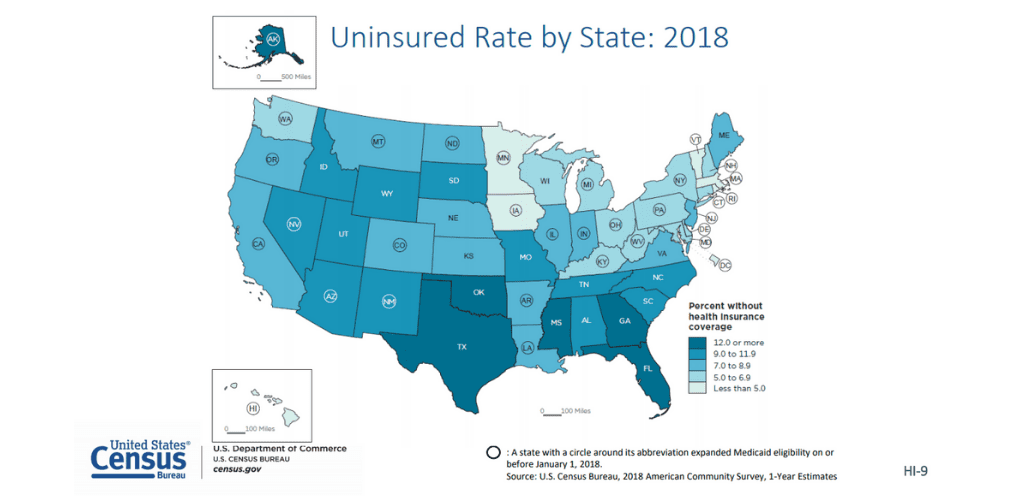
The U.S. Census data released the latest numbers of Americans without health insurance today, and as earlier polls predicted: both the number and percentage of Texans without health coverage got worse for the second year in a row. New U.S. Census data shows the number of uninsured Texans in 2018 was 5 million—186,000 more than in 2017. Texas enjoyed three straight years of historic improvements in our uninsured rates from 2014 to 2016, but lost ground in 2017 and 2018, leaving 17.7 percent of Texans uninsured, the worst Texas rate since 2014.
With two consecutive years of setbacks in 2017 and 2018, Texas remains the state with both the largest number and percentage of uninsured residents in the United States. Inaction by the state leadership and legislature is responsible for Texas’ extreme ranking, while federal actions have also directly undermined coverage across the nation.
One obstacle to Texans demanding real solutions: 2018 polls found that most Texans don’t know the uninsured rate in Texas is higher than other states—let alone that we have been ranked worst for many years. Just over one-third (34 percent) knew that Texas’ uninsured rate is higher than other states (in fact, it is highest in the U.S.). Another 19 percent of those polled thought Texas’ uninsured rate was about the same as other states, and 16 percent thought it was actually lower than most other states.

While the September 10 data release announced a significant increase in uninsured children nationwide, the Census did not release detailed state-specific uninsured statistics for children (or other age groups); those will be provided on September 26, 2019—stay tuned for an update then, with a special focus on children!
Solutions for Texas Adults
Texas has the most limited Medicaid coverage of adults in the nation. Just under one third (about 1.5 million out of 5 million) of uninsured Texans are adults who would gain health coverage if Texas finally accepted an estimated $8-$10 billion a year in federal funds and offered that coverage. States like Texas without any form of Medicaid expansion have no subsidized coverage for working-poor adults because the Affordable Care Act (ACA, or Obamacare) subsidies are only available above the poverty line. The Census report calls attention to the concentration of high uninsured rates among the 14 states that have not yet provided Medicaid to parents and other low-income adults. Much lower uninsured rates in the 34 states with various models of Medicaid expansion also underscore what a powerful tool that policy would be to help cure Texas’ last-place uninsured ranking.
Texas adults with low and moderate incomes also need help from Congress to make commercial insurance affordable for families with incomes above the ACA subsidy income limits. A range of policies of the Trump administration have increased their premiums and deductibles, and also made it harder to enroll in coverage.

Texans Want Action from the Legislature
In 2019 polling, 91 percent of Texans said the state should play a role in a functioning health care system. Similarly, 82 percent of Texans said that the federal government has a similar role in the health care system, and 88 percent say they think health insurance companies should be required to provide coverage for people with pre-existing medical conditions. And, more than half (54%) of Texans say the state should increase spending on health care—only spending on public education (69%) ranks higher.
The state legislature and governor can do better by accepting billions in federal funds to cover working poor adults, and taking steps to stabilize our state insurance markets. Congress can reverse destructive federal policies that are driving down insurance coverage for middle-income Americans, and causing hundreds of thousands of U.S. citizen children to forego health care they deserve. Political pressure fuels action, so Texans who want to see Austin and Washington’s lawmakers do more will need to demand change to reduce the number of uninsured Texans!
Background: Today’s data from the Census Bureau’s American Community Survey—with a massive sample size of about 3.5 million people across the U.S.—confirm with a much higher degree of accuracy what earlier, smaller-sized surveys had predicted. For more information or to schedule an interview with a CPPP expert please contact Oliver Bernstein at bernstein@cppp.org.
Stay tuned as on September 26 the Census Bureau will release more American Community Survey data, including Texas-specific details on the uninsured, and data about poverty and income. To better understand the difference between the two American Community Survey (ACS) and the Current Population Survey (CPS), view our side-by-side comparison.

In June 2018, the Dallas Morning News began publishing a series of in-depth investigative reports on Texans harmed through Medicaid managed care, potential conflicts of interest, and weaknesses in oversight and enforcement of Medicaid managed care contracts. The articles resulted in public hearings in the Texas House of Representatives that further explored the issues and allowed the public to comment.
In response, Texas’ Medicaid agency announced 90 new hires for Medicaid managed care, and conversations among consumer advocates, providers, health plans, and the agency were set in motion. As Texas’ 2019 legislative session approached, it was clear that meaningful reforms were needed to ensure kids, pregnant women, seniors, and people with disabilities in Texas Medicaid get the health care they need.
Public interest advocacy related to Medicaid managed care is layered with challenges: complex policy, equally complex politics, and massive profits—over $450 million netted by Texas Medicaid managed care health plans in 2018—that bring the plans political power and lobbying capacity. In Texas, Medicaid managed care launched over 25 years ago, and is the only version of Medicaid that most lawmakers have ever known. And in those 25 years, struggles between health care providers and Medicaid managed care insurance plans (MCOs) have been a constant. Public interest advocates have to speak loudly to be heard over the clashes between these titan interests.
In Texas, a diverse group of advocates has worked hard to leverage the attention of media and lawmakers, respond to legislators, coordinate testimony, educate lawmakers, and communicate with health care provider associations committed to Medicaid managed care reforms.
When the legislature convened in 2019, more than 50 bills directly related to the issues raised by the Dallas Morning News and the public hearings were filed. A much smaller number passed into law, but they signal major steps forward.
Some high-level reforms that Texas adopted:
New “External Medical Review” option when a doctor-ordered treatment or health service is reduced or denied by a Medicaid managed care insurer (MCO). Today, when a MCO denies or reduces care, the MCO’s “internal appeal” process is not transparent for either the patient or the medical provider recommending treatment. The only next step available today is a federally-required Medicaid fair hearing, but the decision-makers in those hearings don’t have the medical training to analyze whether the services prescribed are medically necessary, nor are they trained on the “functional needs” that allow Medicaid beneficiaries to qualify for long term services and supports.
Going forward, Texas Medicaid will establish a system of independent external reviews that beneficiaries can request, modeled in part on the independent external reviews long available under state law to Texans with private health insurance, and the newer federal external review process established under the ACA. The external medical review will help Medicaid enrollees get an objective, unbiased review of a medical necessity determination, with reviews performed by clinical staff with education and practice in the same or similar area as the health service in question.
“Prior Authorization” (PA) reforms: Reducing barriers and red tape between enrollees and the care they need. Most denials or reductions of care come about when a care provider requests “prior authorization” (PA) from the MCO for a medication, course of treatment, procedure, or medical equipment for a Medicaid enrollee. Texas physicians made reforming Medicaid Managed Care plans’ PA processes their top priority. Now, under the passed measures:
- PA denial notices to enrollees and providers must provide clear reasons, and explain the exact steps needed to gain approval.
- Every Texas Medicaid MCO will have to publicize all of its PA requirements, including the documents and standards a health provider needs to submit to gain authorization. This greater transparency should make it much more likely that a care provider can submit all the documentation needed to get authorization on the first try.
- Texas Medicaid MCOs must conduct an annual review/update of their PA requirements. This step will shed light on any MCOs which have PA requirements that are outliers, not supported by medical research, or conflict with federal or state policy.
“No Wrong Door” for complaints, troubleshooting. Texas law has required a “help line” for Medicaid Managed Care enrollees for over 20 years, but the new laws aim to raise the bar for providing help to enrollees. Texas Medicaid is directed to harness the power of tracking records of complaints, appeals, denials and corrective actions to improve both support for beneficiaries and MCO accountability. Complaints will be aggregated regardless of the source whether from enrollee contacting the Medicaid agency’s managed care helpline, or a legislator’s office calling on behalf of a constituent.
Special protections for kids in foster care, children with disabilities, and medically fragile kids. Texas has moved aggressively to include children in state custody, kids with SSI disability-based Medicaid, and the sub-groups of both of those categories who have medically complex conditions into Medicaid managed care plans in recent years. The most shocking revelations in the Dallas Morning News reporting series and the legislative hearings that followed involved medically fragile children and other children with disabilities.
This focus and the relentless, organized advocacy by parents of medically fragile children yielded many important policy gains. They include:
- A special hotline for children who are medically dependent or have multiple disabilities
- Better coordination between Medicaid and private insurance for kids who are enrolled in both, including better access to medications and specialty care
- Piloting consumer-directed options, accountable care organizations, and other models promoted by the federal Center for Medicare & Medicaid Innovations
Slowing down on Medicaid managed care for individuals with intellectual and developmental disabilities. Despite the warning signs from Texas’ troubled roll-out of Medicaid managed care for foster children and children with disabilities, Texas law still called for moving Medicaid recipients with intellectual and developmental disabilities (IDD) into MCOs in 2021.
New laws passed this session, however, detail a more thoughtful plan to amend that timeline in favor of a pilot program with voluntary participation based on consumer preferences, least restrictive settings, and consumer direction. They also include guardrails for experimental rate methodologies, a comprehensive inventory of benefits, articulated goals, and meaningful evaluation. Statute still identifies plans to move individuals with IDD into MCOs between 2027 and 2031, but the agency is given specific authority to delay deadlines as needed to protect access to services and supports.
Still, many consumer protections initially in legislative proposals did not make it to the finish line.
The newly passed Medicaid managed care reforms above are certainly worth celebrating. Yet, some ambitious proposed consumer protections did not survive the contentious legislative process. Some examples of proposals that did not pass include:
- A comprehensive requirement that would have imposed financial penalties (“liquidated damages”) on MCOs when they fail to comply with their contracts; and a public record of the enforcement actions.
- A requirement that every MCO make medical staff available every day (including early morning and evenings, and for limited hours on weekends and holidays) to allow physicians to consult on prior authorizations for medical care.
- Analysis by Texas’ independent External Quality Review Organizations (EQRO) of the aggregate track records created from MCO inquiries, complaints about access, grievances, denials, appeals, overturned denials, and fair hearings, including comparing the track records of both for-profit and non-profit MCOs.
- Automatic continuation of the health service or treatment that an MCO proposes to deny or reduce, pending the outcome of all appeals, reviews, and fair hearings.
- An online tracking system to allow Medicaid enrollees to follow the status of their appeal to an MCO relayed to a reduction or denial of benefits.
Fortunately, Texas’ Medicaid agency has been planning ahead for expected new reform laws, and early indications are that the agency is moving ahead quickly with new approaches. These include an expanded role for a statewide Medicaid managed care advisory committee, and a strong plan for building the “no-wrong door” model. They plan to keep records of all complaints resolved during the initial contact with the agency (to identify areas for improvement), and have made a new commitment to track all complaints through final resolution.
Texas’ legislative session ended in May 2019 with a major legislative success for kids and families. Implementation of many reforms will require the Medicaid agency to develop new rules, amend the agency’s contracts with MCOs, and seek federal approval for some changes.
Ultimately, fulfilling the promise of reform will depend on the strength of the Medicaid agency and Texas elected officials to enforce new standards. Realizing the promise of reform truly will take a village. Advocates for Texas children, families, people with disabilities, and seniors must continue the drumbeat, insist on steady progress, and push for robust implementation in the months and years ahead.
This piece was written by Anne Dunkelberg, who serves as the CPPP Associate Director/Health & Wellness Team Director, and Adriana Kohler, who serves as Senior Health Policy Associate for Texans Care for Children. See the original publication from the Center for Children & Families (CCF) of the Georgetown University Health Policy Institute.
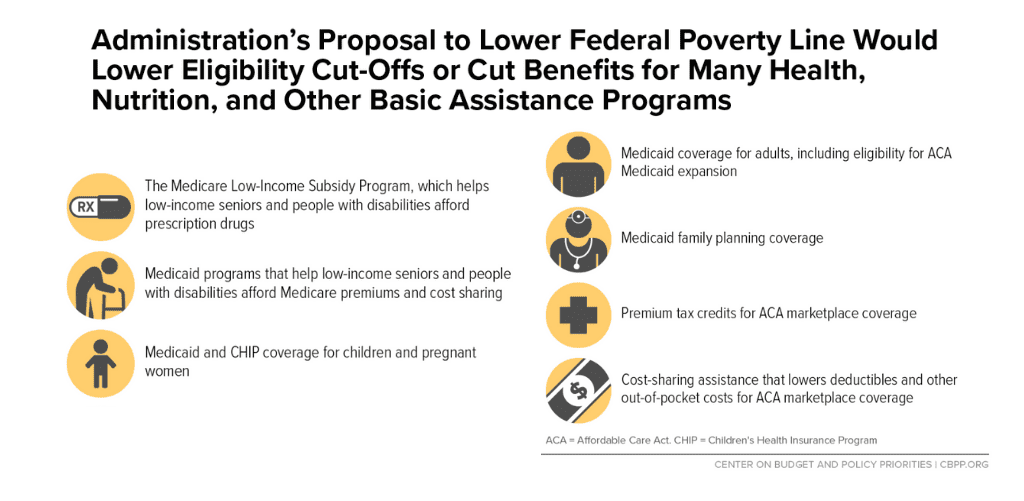
Misguided numbers trick would “move the goal posts” and reduce health care, food, housing benefits and more for millions of Americans
Update: Read CPPP’s Public Comment Opposing the New Federal Proposal that would redefine U.S. Poverty Line
Overview: The U.S. Office of Management and Budget (OMB) issued a notice on May 6 requesting comments on changing the way annual inflation updates are calculated for the federal poverty line. OMB is seeking public comments on the idea of using one of two alternative, lower measures of inflation than the current measure.
Many basic needs programs that work with low-income people use the poverty guidelines as their eligibility thresholds, which are updated annually based on inflation. This new proposal would lower the dollar amounts of those updated poverty thresholds going forward, resulting in fewer low-income American households qualifying for help, or families getting reduced help from those programs. With each additional year of a smaller inflation update under the proposed change, the loss of services for Americans would grow.
Affected programs would include: The Supplemental Nutrition Assistance Program (SNAP, formerly known as food stamps); School meals; the Special Supplemental Nutrition Program for Women Infants, and Children (WIC); Medicaid and the Children’s Health Insurance Program (CHIP); Medicare help with premiums, co-payments and prescription medications; Affordable Care Act Marketplace assistance with premiums and out-of-pocket costs; family planning, home energy assistance; Head Start; Community and Migrant Health Centers; AIDS drug assistance; the Job Corps; the Community Services Block Grant, and legal services for the poor.
Take Action: Submit comments via this online portal before the June 21s deadline. Tell the OMB you oppose this rule change.
Then, help forward this information to more Texas organizations and communities to encourage them to comment.
Who Should Comment:
- Local and state elected officials and local health and human service agencies: if regulators use this change to reduce federal support for services, local governments will be left to fill the growing gap in unmet needs.
- Health care and social service providers, and their associations
- Food banks, food pantries, and other anti-hunger programs
- School districts and boards
- Advocacy organizations concerned with health care, hunger, poverty, child care, access to justice
Important Topics to Include in Comments:
- Directly address the OMB claim that the poverty level income guidelines today are more than adequate, and that they need to grow more slowly. Comment on the evidence from your work that the current federal poverty income guidelines are already well below what it takes to support a family, and that shrinking the inflation update will make the poverty guidelines an even less accurate measure of need.
- Tell OMB that before making a change that will result in a lower poverty income threshold, they must first do extensive research and in-depth analysis, including taking public comments, on: the numbers and types of Americans affected; safety, health, and developmental impacts; impacts on school districts; the fiscal impacts on households and local governments; and other impacts you expect to see among your constituents or the families you serve. (Why? OMB specifically stated that they are not seeking comments on how lowering the poverty guidelines would affect programs that use those guidelines. They are contemplating making this change without researching the impact first. Your comments can show that you expect major impacts on families and your community, and can call on the federal government to do that analysis before making this change.)
How to submit your comments:
- You can use this portal created by the Coalition for Human Needs; or
- Email your comments, addressed to: Nancy Potok, Chief Statistician, Office of Management and Budget, to Statistical_Directives@omb.eop.gov, using “Directive No. 14” in your subject line.
Why Comment?
This OMB request for comments is not part of an official rule-making proposal, so the requirements for taking public comments into account or responding to them are not as clear as for proposed rules. But diverse comments in the public record can achieve these important ends:
- Publicize the impact on people: loss of health, nutrition or other assistance. Comments can show who would be denied assistance, such as children, minorities, seniors, or people with disabilities.
- Question the validity of proposed changes to the inflation index: The Trump Administration has highlighted a specific alternative inflation adjustment, called the Chained Consumer Price Index for Urban Consumers (C-CPI-U). It rises about three-quarters of a percentage point more slowly than the measure now used to adjust the annual poverty measure. Research has indicated that the Chained CPI may not be valid for people who are poor or near-poor.
- Point out that any attempt to measure poverty accurately needs far more than a change in the inflation adjustment; it should take into account current estimates of income and expenditures. It should also take into account the evidence that people with incomes now defined as above the poverty threshold suffer considerable hardship (food insecurity, little or no savings, falling behind in rent or other bills, etc.)
- Raise questions that can be influential with important policy-makers or with the courts: Key members of Congress may weigh in with the Trump Administration to persuade them of the harm of such a change or work to prevent it via legislation. If there is litigation around changing the inflation adjustment, comments may guide court decisions.
More background reading, and answers to your questions:
- Coalition for Human Needs’ poverty line campaign page here, and
- Guide for leaving a detailed, high-quality comment here.
- Here is the 2-page FAQ on the Administration’s Proposal to Lower the Federal Poverty Line: https://www.chn.org//var/www/stage/everytexan.org/html/wp-content/uploads/2019/05/General-Poverty-Line-FAQ.pdf
- From the Center on Budget and Policy Priorities:

Will the reforms survive to become law this Legislative session?
Legislation to improve health care for Medicaid participants and improve insurer performance and accountability is at risk of failing to become law due to late-hour conflicts and legislative process delays. Will all the extensive analysis, public hearings, and negotiations over the last nine months to develop improved policies have been a waste?
Lawmakers filed over 50 bills aimed at reforming Texas Medicaid Managed Care this legislative session, and many had public hearings in April. Today, some clear frontrunners have emerged, but we remain a long way from final decisions about which bills will pass and which reforms will survive the process. Health care provider and health insurance industry associations have put in long hours lobbying for their respective goals and priorities, and the consumer advocates have added their two cents wherever possible.
Notably, several substantial agreed-to policy proposals emerged from a working group of physician, hospital, and insurer lobbyists. While disagreements on other important issues remain, some fundamental improvements have come out of this work. These include the implementation of a new independent medical review option to which participants and providers can appeal denials and reductions of care made by Medicaid Managed Care plans (often referred to as MCOs). There also seems to be consensus around robust new transparency and accountability requirements for MCO “Prior Authorization” requirements before people can access a service. If those two general concepts survive the hectic last month of this legislative session relatively intact, there will be meaningful progress. Advocates for Texans with disabilities and medically fragile children have made important expert contributions to the development of bills.
A number of critical proposed consumer protections for Texas’ 4 million Medicaid participants are in the bills that are “moving.” This post and policy brief looks at five bills. HB 2453 by Sarah Davis, HB 4178 by James Frank, and SB 1105 by Lois Kolkhorst are lengthier bills that cover multiple Medicaid Managed Care topics. HB 3721 by Joe Deshotel and SB 1140 by Kirk Watson (joint authors Hinojosa and West) are single-topic bills to create the new independent medical review option for denials and reductions of care. However, HB 2453 and HB 4178 each also contain provisions to establish the independent medical review function. Together these bills include important proposals on these fundamental Medicaid Managed Care reform topics:
- New Independent Medical Review option, to appeal denials or reductions of care by MCOs, or eligibility denials by HHSC based on medical necessity or functional need
- MCO Accountability: tracking and creating public records of complaints, appeals, denials and corrective actions
- Issues for STAR Kids (children with disabilities and medically fragile kids) and STAR Health (kids in foster care, which includes some medically fragile children)
- Care Coordination Transparency and Adequacy
- “Prior Authorization” (PA) Reforms: Reducing Barriers and Red Tape between enrollees and the care they need.
- Improved Benefits, Network Adequacy, and Quality
- Provisions to Improve the Medicaid Managed Care Provider Experience
Details on each of these topics and the bills are summarized here, beginning with the proposals for an independent medical review option.
Put simply, to get the best protections for Texas Medicaid, the Legislature will need to incorporate provisions from several bills: no single bill currently delivers all of the needed consumer protections. The 86th Legislature has just a few short weeks to get the job done to protect 4 million Texans and the integrity of our public investment in Medicaid Managed Care.
Note: “MCO” stands for Managed Care Organization. All Texas Medicaid Managed Care health plans are licensed as HMOs, but “MCO” is a term used nationally in Medicaid, in order to be inclusive in states where HMOs are not the only vehicle for Medicaid Managed Care delivery.