More than 10 percent of Texas children lack health insurance, giving Texas the worst uninsured rate for children in the country. Our state legislative session is now more than halfway over, and lawmakers have yet to pass any meaningful legislation to address this problem.
The good news is that House Bill 342 by Rep. Philip Cortez and Senate Bill 637 by Sen. Judith Zaffirini would fix a problem with children’s Medicaid enrollment that could greatly improve children’s health insurance rates in Texas. The bills would provide children with continuous eligibility for the entirety of their year-long certification period in Medicaid.
This is the best step Texas can take to reach the estimated 350,000 or more uninsured children who are eligible for Medicaid or the Children’s Health Insurance Program (CHIP) but who are not enrolled.
There and Back Again
Continuous eligibility in children’s health programs is widely recognized as a best practice, including in Texas. But the rules have changed many times over the last few years, creating confusion and denying coverage to kids. Going back to old eligibility policies that have already proven unworkable is costly for the families whose children lose health care coverage due to unnecessary red tape. The old policies are also costly for health care providers and for all Texans.
When the Texas Legislature created CHIP in 1999, all children who were part of CHIP were eligible for 12 months of ongoing care, up until their next annual renewal. CHIP enrollment shot up to half a million children in less than two years after launching! But at that same time, children in Medicaid were still only eligible one month at a time, and risked losing coverage throughout the year.
Families of children in Medicaid—who have lower income than CHIP children—were required to report any income increases that might affect eligibility immediately. Small temporary income increases (like in a month with five payday Fridays) knocked children off Medicaid routinely, and in-person renewal requirements made it hard to get kids back on health care. On average, children only received four months of Medicaid at a stretch, and only a small fraction got a year of health care coverage without any gaps.
Recognizing the success of CHIP’s family-friendly policies, the 2001 Legislature updated Medicaid policy to be more like CHIP: allowing children six months of continuous eligibility followed by a renewal, and allowing their parents to apply and renew a child’s coverage by mail. Children’s Medicaid was transformed, and within two years Medicaid and CHIP had become a stable source of care for more than a third of Texas children.
In the 2003 budget crunch, the Legislature shortened continuous eligibility in CHIP from 12 months to six months. In 2007, the Legislature recognized the importance of 12 months of continuous eligibility in keeping children healthy and restored it for CHIP but left children’s Medicaid with 6 months of continuous eligibility followed by a renewal, and then another six months of continuous eligibility.
In 2014, updated federal Medicaid rules designed to eliminate red tape barriers required every state to have no more than one formal renewal of children’s coverage per year. In implementing this change, the Texas Health and Human Services Commission (without legislative input or direction) created an entirely new policy, eliminating continuous eligibility in the second six months of each child’s 12-month certification period. This change returned children’s Medicaid coverage to the old pre-2002 month-to-month coverage policy for the second half of each year. In addition, the agency introduced a new system of “Periodic Income Checks” (PICs) that check family income at months five, six, seven, and eight. The unfortunate results soon became evident.
Where There’s Smoke, There’s Fire
Since the implementation of the new policy for Children’s Medicaid in 2014, Medicaid managed care plans, providers, and community-based organizations have received a steady stream of reports of families getting overloaded with confusing letters and requests from the Health and Human Services Commission for information. Many of these families eventually lost coverage because they didn’t know what response was required of them or were unable to respond in the very narrow timeframe provided. Families have 10 days from the date the system generates a request (which is not necessarily the same day it is mailed) to respond. Unfortunately, many families receive this notice too late to return the required information before the deadline.
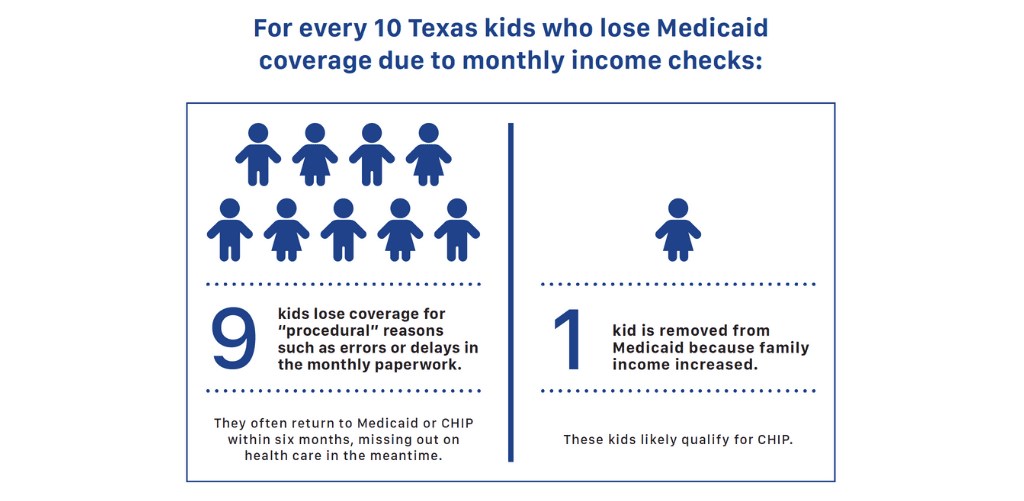
Recent data released by HHSC has substantiated reports from providers and community-based organizations. According to this data, HHSC reaches out to an average of 6,471 families each month as a result of periodic income checks. Of those contacted, 1,932 on average are able to confirm that their family is in fact not over income. This shows that the databases and income check process are wrong at least 30 percent of the time (1,932 out of the 6,471). On average, only 372 children are actually confirmed to be over income. The remaining 4,162 children are denied because the required verification was not received within the very short timeframe.
This means thousands of Texas children fall through the cracks because of red tape every month.
A total of 47,014 children in 2017 and a total of 52,875 children in 2018 were kicked off Medicaid simply for excessive bureaucratic hurdles.
Notably, about 40 percent of the children who
Many Kids lose Medicaid each month because of paperwork and red tape

Let’s Go Back to Best Practices and Common Sense
The policy changes that HHSC implemented in 2014 essentially returned the Texas Medicaid program for children to pre-2002 policies that were inefficient and costly. The old pre-CHIP policy is costly for the families whose children lose health care coverage due to unnecessary red tape. The old policy is also costly for our Medicaid Managed Care program as it undermines initiatives aimed at reducing the overall cost of the program. And the policy is costly for Texans and hospitals who bear much of the cost when avoidably uninsured children have no choice but to seek care in emergency rooms.
HB 342 by Rep. Cortez and SB 637 by Sen. Zaffirini seek to restore the common-sense policy of providing continuous eligibility in Medicaid for children. The bills would align the children’s Medicaid policy to the policies in Texas CHIP by providing 12 months of continuous eligibility, and eliminating inaccurate and excessive income checks. The Legislature should enact this legislation, which offers a simple, affordable and effective step our state can take to reach the roughly 350,000 uninsured children who are eligible for Medicaid or
TAKE ACTION HERE by urging the Senate Health and Human Services Committee to Vote for Texas Children’s Health!