All Texans deserve high-quality health care, whether it’s for a physical ailment or a mental health or substance use issue.
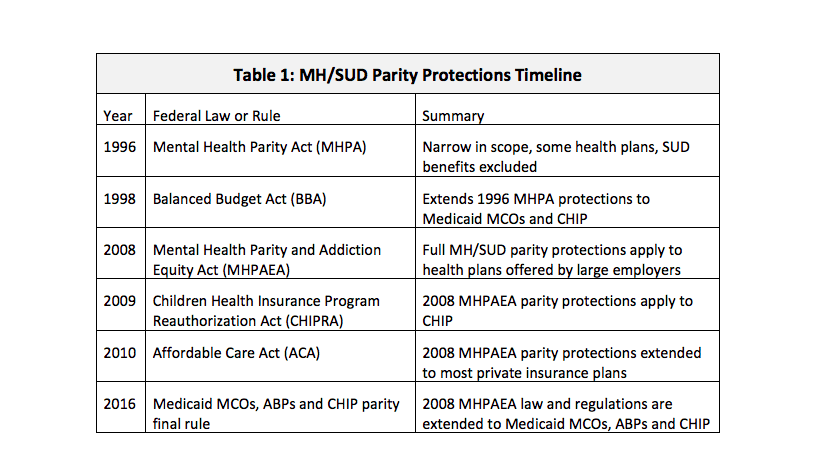
In health insurance, the term “parity” describes the equal treatment of mental health (MH) conditions and substance use disorders (SUD) in insurance plans, when compared to coverage for medical or surgical (M/S) health care. When a plan has parity it means that, for example, if an insurer provides unlimited doctor visits for a condition like diabetes, then the insurer should also provide unlimited doctor’s visits for mental health conditions like depression or schizophrenia.
On December 2, 2017, Texas Medicaid was scheduled to come into compliance with new parity protections required under federal rules. HHSC has created a new web home for this area of policy, and in upcoming reports CPPP will review the newly-posted analyses. This brief explains the new protections and Texas’ process to implement them.
This new CPPP policy brief explains in more detail the key provisions under the federal Medicaid parity rule, and the process of implementation in Texas.
Other Texas Parity Updates
During the 2017 Texas Regular Legislative Session, lawmakers passed an important bill related to mental health parity (House Bill 10). The new law, signed by Governor Abbott, aims to address ongoing challenges with mental health and substance use disorder parity protections for Texans.
HB 10 took effect on September 1, 2017, however the implementation process is ongoing. The legislation addresses parity from four different angles: regulation, data collection, collaboration, and consumer assistance. These different pieces are moving ahead in different stages.
Regulation: the Texas Department of Insurance (TDI) has started enforcing parity requirements as outlined in HB 10 for health plans that will take effect on January 1, 2018.
Data Collection: TDI and HHSC have joined forces to create a data collection tool that insurance companies and managed care organizations will use to collect data required by HB 10, for both commercial and Medicaid-CHIP markets. The agencies accepted public comment on the proposed tool through November 17, 2017. TDI aims to finalize the data collection tool and send it to insurers and MCOs before the end of the year.
Stakeholder workgroup: HHSC has appointed 18 members to its Mental Health Condition and Substance Use Disorder Parity Workgroup established by HB 10. The workgroup is housed under HHSC’s Behavioral Health Advisory Council (BHAC). HHSC convened the workgroup for the first time on November 27, 2017.
Consumer Assistance: The Behavioral Health Access to Care Ombudsman created by HB 10 will be housed at the Office of the Ombudsman at HHSC and serve both commercial and Medicaid-CHIP enrollees. HHSC aims to have the new Ombudsman function in place as of January 1, 2018.
For more information on HB 10 click here.
All Texans deserve high-quality health care, whether it’s for a physical ailment or a mental health or substance use issue. The HHSC parity analysis and MCO changes that may flow from it are important but still very early steps toward eventually realizing the great promise that mental health parity laws and regulations hold. It will be important for all behavioral health stakeholders to monitor and engage in the next steps in implementation of the Medicaid and CHIP final parity rule, to ensure that more Texans gain equal access to mental health and other health care services needed to achieve recovery.
Read more at http://bettertexasblog.org/category/health-care/mental-health/